Your Mop is Holding You Back
Let’s start with one word – clean. What does it mean to be clean? From a scientific perspective, a surface is only clean during the absence of unwanted matter. Unfortunately, according to every scientific study we found or conducted, mops fail to make surfaces clean.
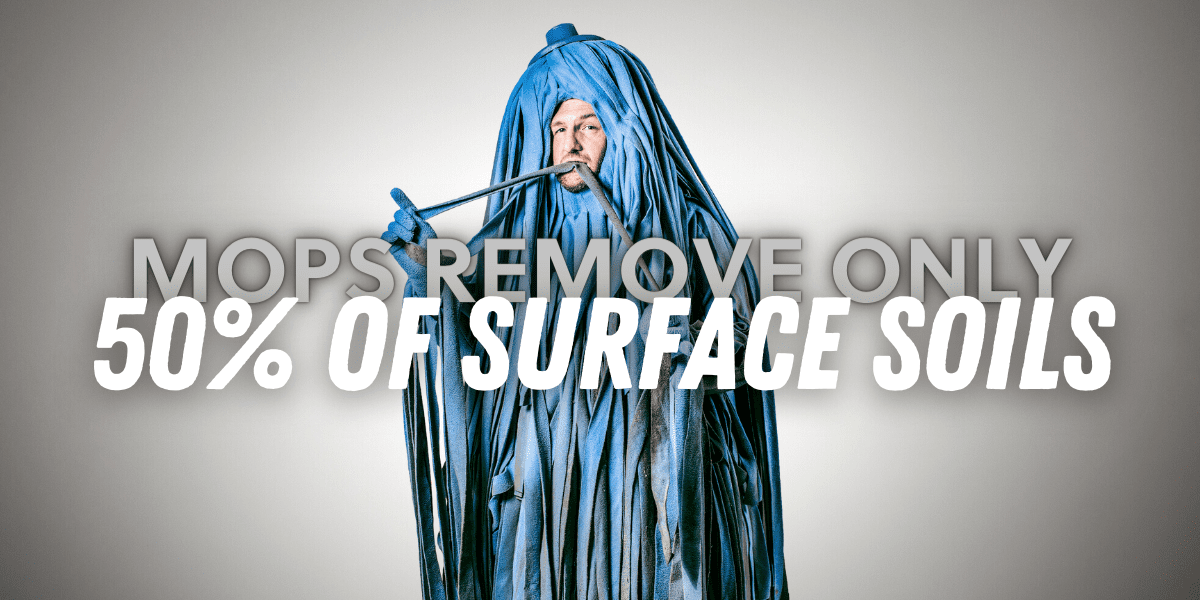
The Disgusting Truth About Mops
-
- A new microfiber mop removes only about 50 percent of surface soils and bacteria. (TURI study on AutoVac 2012; American Society of Microbiology, 1971)
- Mops are actually responsible for bacterial contamination on floors. (Study conducted by Canada’s University of Ottawa)
- “Mops can be a serious potential source of contamination…even when soaked in disinfectant overnight, contaminants could still be detected.” (The Pharmaceutical Journal, March 18, 2000)
- “Mops stored wet supported bacterial growth to very high levels and could not be adequately decontaminated by chemical disinfection.” (Reported in Food Safety and Quality, February 2015)

Floor Care Could Be So Much Better
In order to stop mops and their inferior cleaning, we need superior alternatives. Studies prove that Kaivac technologies remove soil and bacteria and improve the cleanliness and health of hard surfaces.
A Kaivac No-Touch Cleaning system not only cleans fixtures 3 times faster than traditional methods. It also removes 98% of urine residue on both smooth hard surfaces and grout lines. (Source here.) A study at the University of Massachusetts showed that during floor cleaning trials, the Kaivac AutoVac removed 98.3 percent of the available soil, while a brand new microfiber mop on the same floor only removed 50.9 percent of the same soil. The difference is clear. Explore our alternatives to mopping below.
Alternatives to Mopping: Effective Cleaning Systems
UniVac®
In areas with obstacles to maneuver, the UniVac cleans under and around furniture and appliances, leaving floors dry.
AutoVac Stretch™
Improve productivity cleaning wide open areas. The AutoVac Stretch leaves floors clean and dry in a single pass.
Icky the Mop Has Tried to Fight Back Against Our Campaign
Helpful Articles
Stop the Mop to Increase Cleaning Productivity
Everyone knows that mops clean floors…or so they think. In actuality, mops spread dirt and contaminants around instead of actually removing them.
BTG Labs Stopped the Mop With Kaivac Floor Care
To create a welcoming space that earns the trust of large customers, BTG Labs President Tom McLean stopped the mop in his facility. They now use the AutoVac.
How to Clean Commercial Restroom Floors
Often a freshly mopped restroom will start smelling bad before the floor even dries. This is because mopping fails to draw dirt out of the grout.










